Effective Medications for Arthritis Pain Relief: What Works Best?
When managing arthritis pain, various medications can provide significant relief. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, effectively reduce inflammation and pain. Corticosteroids can offer rapid relief for severe symptoms. For chronic cases, disease-modifying antirheumatic drugs (DMARDs) help slow disease progression. Additionally, topical analgesics can provide localized relief. Consult a healthcare professional to determine the best option for your specific needs.
Understanding Arthritis and Its Impact
Arthritis is a term commonly used to describe inflammation of the joints, encompassing over 100 different types, including osteoarthritis (OA) and rheumatoid arthritis (RA). This chronic condition affects millions of people worldwide, leading to significant pain, stiffness, and swelling in the joints, which can severely impact daily activities and quality of life. The management of arthritis pain is crucial for maintaining mobility and overall well-being.
Common Medications for Arthritis Pain Relief
Effective pain management for arthritis typically involves a combination of medications tailored to the type of arthritis, its severity, and the individual patient’s needs. The following categories of medications are commonly prescribed for arthritis pain relief:
1. Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
NSAIDs are among the most commonly used medications for arthritis pain relief. They work by reducing inflammation, which in turn alleviates pain. Over-the-counter options like ibuprofen (Advil, Motrin) and naproxen (Aleve) are widely used, while stronger NSAIDs such as diclofenac and indomethacin are available by prescription.
While NSAIDs can be effective, they also come with potential side effects, including gastrointestinal issues, kidney problems, and increased risk of cardiovascular events, especially with long-term use. Patients should discuss the risks and benefits with their healthcare provider.
2. Acetaminophen
Acetaminophen (Tylenol) is another common pain reliever that can be effective for mild to moderate arthritis pain. It works primarily as a pain reliever and fever reducer but does not have anti-inflammatory properties like NSAIDs. Acetaminophen is generally considered safer for long-term use than NSAIDs, particularly for individuals with pre-existing gastrointestinal or cardiovascular conditions.
However, it is essential to adhere to recommended dosages, as excessive use can lead to liver damage. Patients should consult their healthcare providers to determine the appropriate dosage and duration of use.
3. Disease-Modifying Antirheumatic Drugs (DMARDs)
For individuals with rheumatoid arthritis, DMARDs play a crucial role in managing pain and preventing joint damage. These medications, such as methotrexate, sulfasalazine, and leflunomide, work by suppressing the immune system to reduce inflammation and halt disease progression.
While DMARDs can be effective in managing symptoms, they often take several weeks to show benefits, and patients may experience side effects such as nausea, liver toxicity, and increased susceptibility to infections. Regular monitoring by a healthcare provider is essential during treatment.
4. Biologic Response Modifiers
Biologics are a newer class of DMARDs that target specific components of the immune system. Medications such as adalimumab (Humira), etanercept (Enbrel), and infliximab (Remicade) are examples of biologics used to treat rheumatoid arthritis and other forms of inflammatory arthritis.
Biologics tend to be more expensive than traditional DMARDs but can be highly effective for individuals who do not respond to conventional treatments. They carry a risk of serious infections and other side effects, necessitating careful patient selection and monitoring.
5. Corticosteroids
Corticosteroids, such as prednisone, are potent anti-inflammatory medications that can quickly reduce swelling and pain. They are often used for acute flare-ups of arthritis or when other medications are ineffective. Corticosteroids can be administered orally, injected into the joint, or given as infusions.
While effective, long-term use of corticosteroids can lead to significant side effects, including weight gain, osteoporosis, and increased blood sugar levels. Due to these risks, they are typically prescribed for short durations or in low doses.
6. Topical Analgesics
Topical analgesics, such as capsaicin cream and diclofenac gel, are applied directly to the skin over the affected joints. Capsaicin works by depleting substance P, a neurotransmitter involved in pain perception, while diclofenac gel provides localized anti-inflammatory effects.
Topical treatments can be particularly beneficial for patients who prefer to avoid systemic medications or experience adverse effects from oral medications. They generally have fewer side effects, but their effectiveness may vary from person to person.
7. Alternative and Complementary Therapies
Many individuals seek alternative therapies to manage arthritis pain, either in conjunction with traditional medications or as standalone treatments. Some of the most popular complementary therapies include:
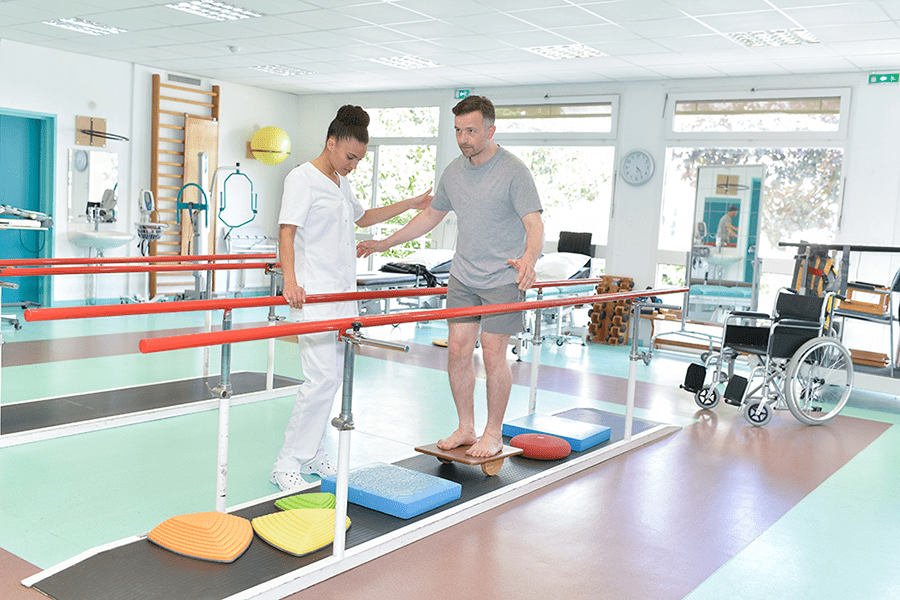
A. Physical Therapy
Physical therapy involves tailored exercises to improve joint function, strength, and flexibility, helping to alleviate pain and improve mobility. A physical therapist can design a specific program based on individual needs and limitations.
B. Acupuncture
Acupuncture, a traditional Chinese medicine practice, involves inserting thin needles into specific points on the body. Some studies suggest that acupuncture may help reduce arthritis pain and improve function, though results can vary.
C. Dietary Supplements
Certain dietary supplements, such as glucosamine and chondroitin sulfate, are popular among individuals seeking natural relief from arthritis pain. While some studies show modest benefits, research results are mixed, and patients should consult their healthcare providers before starting any new supplement regimen.
8. Lifestyle Modifications
In addition to medications, lifestyle changes can significantly impact arthritis pain management. Some helpful strategies include:
A. Weight Management
Maintaining a healthy weight can alleviate stress on weight-bearing joints, particularly in individuals with osteoarthritis. Even modest weight loss can lead to significant improvements in pain and function.
B. Regular Exercise
Engaging in low-impact exercises, such as swimming, walking, and cycling, can help improve joint function and reduce pain. Regular physical activity is essential for maintaining overall health and well-being.
C. Heat and Cold Therapy
Applying heat or cold to affected joints can provide temporary relief from pain and inflammation. Heat therapy can help relax muscles and improve circulation, while cold therapy can numb pain and reduce swelling.
9. Emerging Treatments and Future Directions
The field of arthritis treatment is constantly evolving, with ongoing research into new medications and therapies. Some promising areas of investigation include:
A. JAK Inhibitors
Janus kinase (JAK) inhibitors are a class of oral medications that target pathways involved in inflammation. Drugs like tofacitinib (Xeljanz) have shown effectiveness in treating rheumatoid arthritis and are being studied for other forms of arthritis.
B. Stem Cell Therapy
Stem cell therapy is a novel approach being explored for arthritis treatment. Research is ongoing to determine the safety and efficacy of using stem cells to regenerate damaged cartilage and reduce inflammation.
C. Gene Therapy
Gene therapy holds potential for targeting the underlying causes of arthritis at a molecular level. While still in experimental stages, advancements could lead to more personalized and effective treatments in the future.
Conclusion
Effectively managing arthritis pain requires a comprehensive approach that includes medications, lifestyle modifications, and possibly complementary therapies. While various medications are available, the best treatment plan will depend on the individual’s specific type of arthritis, overall health, and personal preferences. Collaboration with a healthcare provider is essential to determine the most effective strategy for pain relief and to monitor for any potential side effects. With ongoing research and advancements in treatment options, there is hope for improved pain management and quality of life for those living with arthritis.
Explore
Event Planning Software for Small Teams: Affordable and Effective Options
Finding Freedom: A Comprehensive Guide to Effective Urinary Incontinence Treatments

Top Online Therapy Platforms for Depression Support
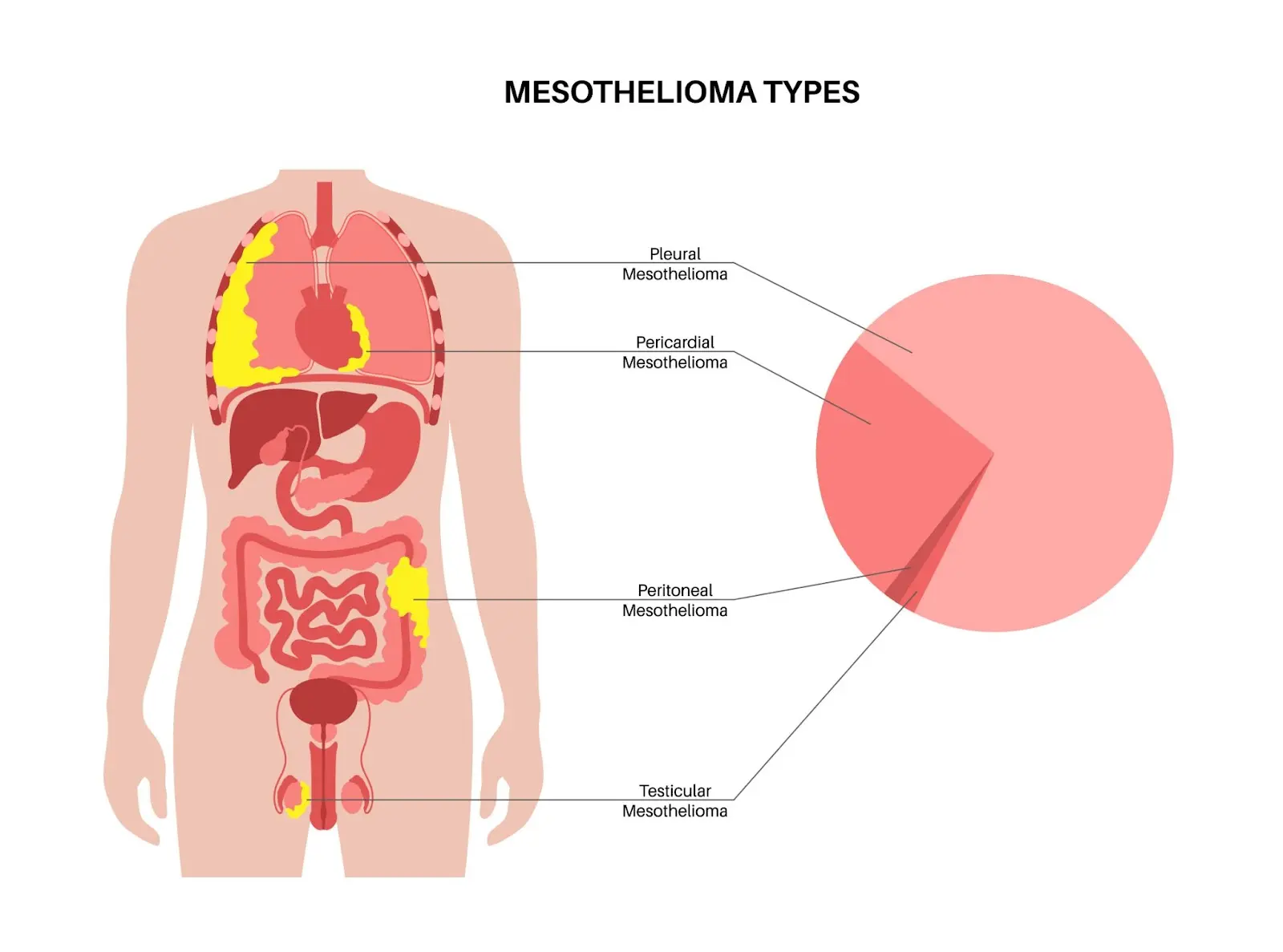
Mesothelioma Treatment Options: What Patients Need to Know

Choosing the Right Health Insurance Plan: A 2025 Guide

Understanding Childhood Asthma: Symptoms, Causes, and Treatment Options

How Sewer Cameras and Locators Improve Plumbing Diagnostics
Selecting the Best Rehab Center: Key Factors to Consider
